Introduction: The Persistent Challenge of Hyperpigmentation
Imagine finally clearing a stubborn breakout, only to find a dark mark taking up residence long afterward. Or spending a pleasant weekend outdoors and discovering new sunspots appear as unwelcome souvenirs. Such experiences reflect the complex, persistent challenge of hyperpigmentation—a common skin disorder that affects millions worldwide. Far beyond a surface issue, hyperpigmentation signifies deeper skin dysfunction, involving molecular and cellular processes triggered by a combination of genetic, environmental, and hormonal factors. This guide dives deep into the science behind the causes of hyperpigmentation, debunks common myths, and sheds light on advances shaping safer, more effective treatments.
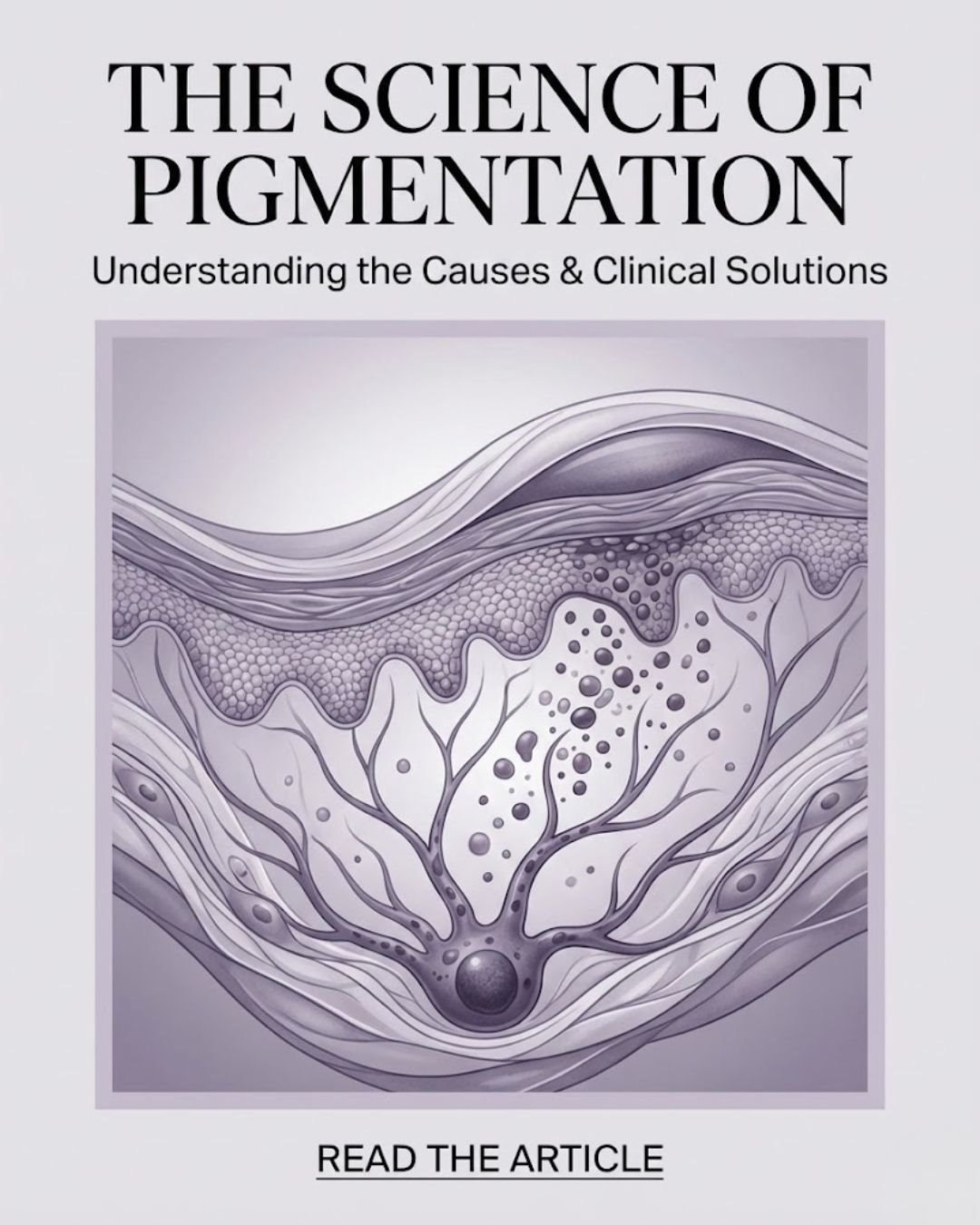
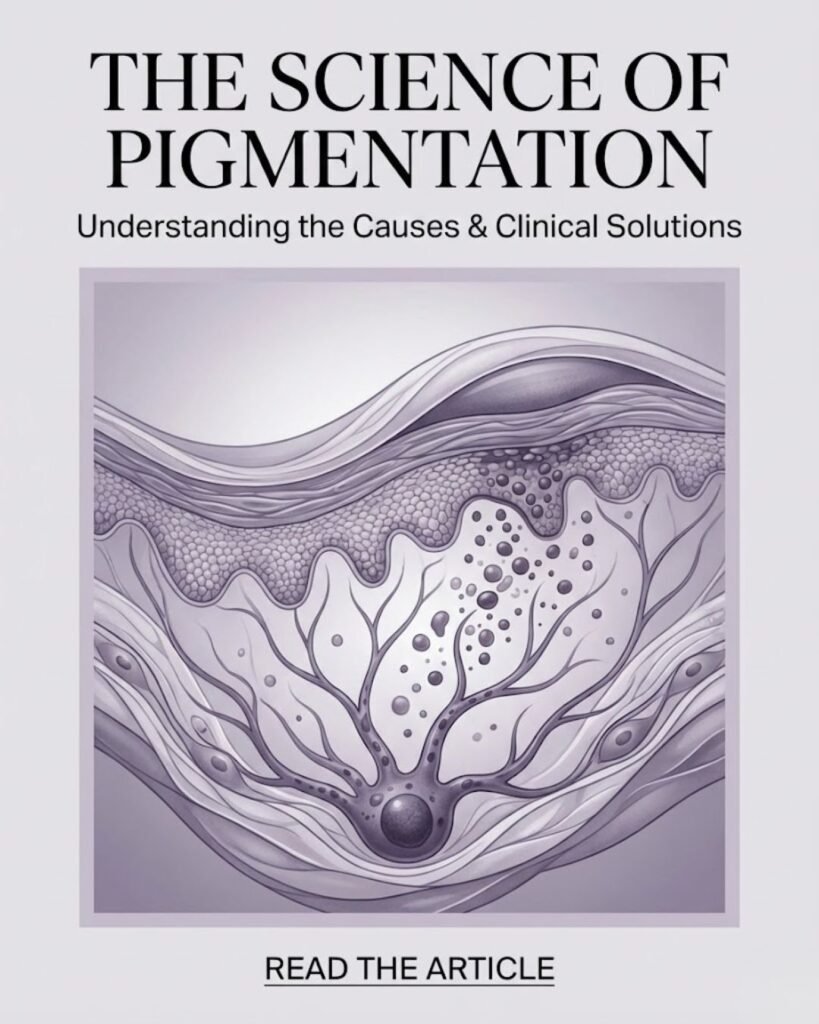
The Biology of Pigment Production: Meet the Melanocyte
The Melanocyte: Skin’s Tiny Octopus
At the cellular heart of pigmentation lies the melanocyte, a fascinating cell tucked away in the basal layer of the epidermis. Named for its tentacle-like dendrites, a single melanocyte connects with approximately 30 to 40 keratinocytes, supplying each with melanin-filled melanosomes.
Melanin: Nature’s Sunscreen
Melanin, a complex polymer, imparts color to our skin, hair, and eyes. It is produced in response to ultraviolet (UV) radiation exposure. UV rays activate a signaling cascade prompting melanocytes to synthesize melanin, which then absorbs and dissipates the harmful energy, protecting skin DNA from damage.
Micro-Damage and Oxidative Stress: The Culprits of Persistent Spots
Prolonged UV exposure and pollutants generate free radicals, highly reactive unstable molecules. These free radicals impair key cellular structures causing oxidative stress and subclinical inflammation—a state termed micro-damage.
Micro-damage activates melanocytes to produce melanin erratically, resulting in splotchy, clumpy pigment deposits visible as dark spots or dull skin.
Fitzpatrick Scale: Who Is Most Vulnerable?
The Fitzpatrick scale classifies skin types based on pigmentation and UV response:
- Types I and II: Fair skin, burns easily, tans minimally
- Types III to VI: Increasingly darker skin tones with more reactive melanocytes
Individuals with medium-to-dark skin types (III–VI) are more predisposed to post-inflammatory hyperpigmentation (PIH), where pigment darkens after skin inflammation or injury.
Common Causes of Hyperpigmentation
1. Ultraviolet (UV) Radiation: The Primary Trigger
The sun’s UV rays, especially UVA and UVB, stimulate melanocytes to increase melanin as a protective measure. Chronic sun exposure leads to:
- Sunspots (solar lentigines)
- Freckles
- Worsening of melasma or existing PIH
UV penetration through clouds and even glass windows means sun protection is critical year-round.
2. Post-Inflammatory Hyperpigmentation (PIH): Dark Marks After Skin Injury
PIH occurs when excess melanin is produced as a response to skin inflammation. Causes of hyperpigmentation include:
- Acne lesions and scarring
- Eczema or psoriasis
- Scrapes, cuts, burns
- Post-procedure irritation (from peels, lasers)
Darker skin types often experience more persistent PIH due to melanocyte hyperreactivity.
3. Hormonal Influences: Melasma and Pregnancy Mask
Fluctuations in estrogen and progesterone levels activate melanocyte melanin synthesis. Melasma, known as the “mask of pregnancy,” manifests as diffuse, brownish patches usually on cheeks and forehead, influenced strongly by:
- Pregnancy
- Oral contraceptives
- Hormone replacement therapy
Sun exposure synergistically aggravates these hormone-driven pigment changes.
4. Genetic Predisposition
Genetics influence melanocyte number, melanin type, and enzymatic activity governing pigmentation. Over 100 genes regulate melanin production and melanosome transport, accounting for individual differences in pigmentation tendency.
Certain inherited conditions (e.g., oculocutaneous albinism) alter pigment biology dramatically but are rare.
5. Skin Aging
With age, melanocytes decrease in number but increase in size and activity, causing uneven melanin distribution. This leads to age spots and solar lentigines characteristic of mature skin.
6. Medications and Chemicals
Various drugs increase pigmentation either by stimulating melanin synthesis or by photosensitizing skin:
- Antibiotics (e.g., tetracyclines)
- Chemotherapy agents
- Oral contraceptives and hormone therapies
- Tricyclic antidepressants
Topical chemicals in cosmetics or treatments causing irritation can also be causes of hyperpigmentation.
7. Underlying Medical Conditions
Rare systemic conditions cause skin pigmentation:
- Addison’s disease: Hormonal imbalances increase melanin, causing dark patches
- Hemochromatosis: Iron overload leads to skin darkening
- Chronic endocrine disorders can similarly disrupt pigmentation homeostasis
Risk Factors Amplifying Causes of Hyperpigmentation
Understanding the risk factors that amplify the causes of hyperpigmentation is crucial for prevention, diagnosis, and tailoring effective treatments. These factors influence the likelihood, severity, and persistence of dark spots and uneven pigmentation.
1. Fitzpatrick Skin Types: Darker Skin Is More Susceptible
The Fitzpatrick Skin Type classification system categorizes human skin into six types based on its response to ultraviolet (UV) light, primarily its tendency to burn or tan. This is essential in dermatology for assessing risk of sun damage and pigmentation disorders.
- Types I to III represent fair to light skin, more prone to burning and sun damage but less prone to persistent hyperpigmentation.
- Types IV to VI, commonly described as olive to deep brown/black skin, have a higher baseline melanin content but more reactive melanocytes.
Why are darker skin types more prone?
- Individuals with Fitzpatrick types IV to VI (darker skin tones) possess more active melanocytes that respond excessively to inflammation or injury, increasing the risk of Post-Inflammatory Hyperpigmentation (PIH).
- Studies show PIH prevalence rates of up to 65% in darker-skinned populations with acne or inflammatory skin diseases.
- The higher melanin production in darker skin, although protective against UV damage, increases persistent pigmentation issues after skin trauma.
Moreover, cosmetic procedures like chemical peels or laser therapies carry a higher risk of triggering unwanted pigmentation changes in these skin types due to deeper or more prolonged skin injury.
2. Female Sex and Hormonal Changes
Females are at a greater risk of developing specific types of hyperpigmentation, mainly due to hormonal influences:
- Melasma predominantly affects women, particularly during pregnancy (the “mask of pregnancy”) and with oral contraceptive or hormone replacement therapy use.
- Hormonal fluctuations stimulate melanocytes, increasing melanin synthesis and enhancing the visibility of dark patches.
- Women may experience cyclical pigmentation changes related to their menstrual cycle due to hormonal shifts.
Though men can develop hyperpigmentation, hormonal causes are a significant risk amplifier for women.
3. Excessive Ultraviolet (UV) Exposure Without Protection
UV radiation remains the most potent environmental trigger:
- Both UVA and UVB rays stimulate melanocyte activity, promoting melanin production as a defense mechanism.
- Lack of daily broad-spectrum sunscreen use doubles down on risk, allowing chronic UV-induced damage and persistent pigmentation.
- UVA rays penetrate glass and clouds, making sun protection critical even on overcast days or indoors near windows.
- Cumulative sun exposure can cause solar lentigines (age spots), freckles, and worsen existing hyperpigmentation including melasma and PIH.
Regular sun exposure without protection not only initiates new hyperpigmentation but perpetuates existing dark spots.
4. History of Inflammatory Skin Conditions
Chronic or recurrent inflammation significantly amplifies pigmentary risk:
- Diseases such as acne vulgaris, eczema, psoriasis, and dermatitis cause repeated skin injury and inflammation.
- Inflammatory mediators signal melanocytes to overproduce melanin.
- In individuals prone to hyperpigmentation, even minor irritation can provoke persistent dark spots.
- PIH resulting from inflammation tends to be more severe and lasting with increased frequency and depth of inflammatory episodes.
Managing underlying inflammatory conditions is essential in reducing hyperpigmentation exacerbation.
5. Improper Skincare Causing Irritation or Trauma
Skincare habits can unintentionally increase pigmentation risk:
- Over-exfoliation, harsh scrubs, and aggressive physical removal damage the epidermal barrier and cause microscopic tears.
- Use of irritating or allergenic products triggers inflammation, further stimulating melanocyte activity.
- Picking or squeezing acne lesions results in localized injury, greatly increasing post-inflammatory hyperpigmentation, especially in darker skin tones.
- Inappropriate use of chemical peels or treatments without professional guidance can cause pigmentation worsening.
Myths Dispelled: What Doesn’t Address the Causes of Hyperpigmentation
Scrubbing Away Spots
Many believe that aggressively scrubbing the skin can remove dark spots. However, physical scrubbing damages the skin barrier and causes micro-tears and inflammation. This inflammation triggers melanocytes to produce excess melanin, worsening existing pigmentation or even causing new dark spots. Gentle cleansing and exfoliation with scientifically supported products are far safer and more effective.
Lemon Juice as a Natural Remedy
Lemon juice is often touted as a natural brightener, but it is highly acidic and phototoxic. Applying lemon juice can lead to severe chemical burns when exposed to sunlight, a condition called phytophotodermatitis. This reaction not only damages skin but often results in lasting dark marks, exacerbating hyperpigmentation rather than improving it. Dermatologists recommend avoiding lemon juice and instead using clinically tested ingredients.
Tingling Sensations Equals Effectiveness
Some users associate a tingling or burning sensation during product application with treatment efficacy. In reality, tingling often signals irritation and compromised skin barrier function. Irritation provokes inflammation, which activates melanocytes and worsens hyperpigmentation. Effective products aim for gentle, non-irritating formulations that strengthen the skin barrier while lightening pigment.
Skipping Sunscreen on Cloudy Days
A common misconception is that sunscreen is unnecessary when it’s cloudy or indoors. Up to 80% of UVA rays—the primary contributors to skin aging and pigment stimulation—penetrate clouds and glass. Neglecting sunscreen during these conditions allows UV radiation to persistently activate melanocytes, leading to worsening of existing spots and formation of new pigmentation. Daily, broad-spectrum sunscreen is essential regardless of weather or indoor/outdoor settings.
Preventing Causes of Hyperpigmentation: The Most Effective Strategies
Prevention remains the cornerstone of managing hyperpigmentation since treatment can be lengthy and recurrences common without proper care. Prioritizing prevention helps maintain even skin tone and reduces the formation of new spots.
1. Daily Broad-Spectrum Sunscreen: Your Best Defense
Sun exposure is the leading cause of hyperpigmentation. Protecting skin every day with a broad-spectrum sunscreen that guards against both UVA (ages skin) and UVB (burns skin) rays is essential.
- Choose sunscreens with SPF 30 or higher.
- Apply generously to all exposed areas 15–30 minutes before going outside.
- Reapply every two hours, more often if sweating or swimming.
- Protect vulnerable areas like lips, ears, and the back of hands with specialized products or clothing.
- Remember UVA rays penetrate clouds and glass windows—protection indoors and on cloudy days matters.
2. Use Antioxidants to Combat Oxidative Stress
Topical antioxidants such as Vitamin C and niacinamide neutralize free radicals generated by UV and pollution, preventing micro-damage and pigment production.
- Vitamin C not only hinders melanin synthesis but also brightens skin tone.
- Niacinamide strengthens the skin barrier and inhibits melanin transfer to the surface, reducing spot visibility.
- Incorporate antioxidant serums into your morning skincare routine for preventive benefits.
3. Gentle Skincare Avoiding Inflammation
Avoid harsh scrubs, aggressive exfoliation, and irritating products which provoke inflammation—a key trigger for hyperpigmentation. Opt for gentle cleansers and mild exfoliants like alpha-hydroxy acids (AHAs) or beta-hydroxy acids (BHAs).
Maintain healthy skin barrier function through adequate hydration and moisturization to reduce susceptibility to pigment issues.
4. Avoid Picking or Squeezing Blemishes
Acne, insect bites, and other skin injuries can lead to post-inflammatory hyperpigmentation if aggravated by picking. Hands-off treatment helps prevent unnecessary inflammation and dark spot formation.
5. Mindful Lifestyle Choices
Chronic stress increases systemic inflammation and can exacerbate pigmentary disorders. Ensuring adequate sleep, balanced nutrition rich in skin-supportive vitamins (A, C, E), and hydration supports skin repair and resilience.
Treatment Options for Hyperpigmentation: From Science to Practice
While prevention is critical, treatment becomes necessary for many to reduce existing dark spots and uneven pigmentation.
Topical Therapies: The First Line of Defense
Topical products typically work by interrupting the melanin production pathway, accelerating skin turnover, or reducing melanin transfer:
- Hydroquinone: A gold-standard tyrosinase inhibitor but with possible irritation and prolonged use risks.
- Niacinamide: A multitasker that prevents pigment transfer and reinforces barrier health with low irritation.
- Azelaic Acid: Decreases melanin production and is anti-inflammatory, suitable for sensitive skin.
- Retinoids (e.g., Tretinoin): Speed up cell turnover and disperses melanin; may increase sun sensitivity.
- Vitamin C: Brightens skin and inhibits melanin synthesis while providing antioxidant protection.
- Kojic Acid and Tranexamic Acid: Tyrosinase inhibitors with varying efficacy; tranexamic acid shows promise in melasma.
Combination therapies often provide enhanced, synergistic results.
Chemical Peels and Exfoliation Treatments
Chemical peels using AHAs (glycolic, mandelic acid), BHAs (salicylic acid), or trichloroacetic acid assist in removing pigmented upper skin layers, promoting regeneration. Peels should be chosen carefully based on skin type and pigmentation severity to avoid irritation-induced PIH.
Laser and Light-Based Therapies
Laser treatments (e.g., low-fluence Q-switched, fractional lasers, Intense Pulsed Light) selectively target pigmented areas for breakdown. These require skilled administration and caution in darker skin tones due to PIH risk.
Emerging low-energy laser protocols and microneedling with topical agents have shown promising efficacy.
Oral Treatments
For resistant hyperpigmentation, oral tranexamic acid is gaining acceptance under medical supervision for melasma and PIH, helping inhibit pigmentation pathways systemically.
NIASORCINOL™: A Revolutionary Multi-Pathway Approach

NIASORCINOL™ represents a breakthrough in pigmentation science, combining multiple active molecules in a patented formulation that addresses hyperpigmentation on several fronts simultaneously:
- Slowing Melanin Production with E-Resorcinol: This stable, potent molecule inhibits tyrosinase activity by blocking the enzyme’s active site, reducing new pigment synthesis.
- Blocking Melanin Transfer with Niacinamide: A well-known vitamin B3 derivative, niacinamide prevents melanosomes from transferring pigment into surface skin cells, fading visible dark spots.
- Clearing Existing Melanin through Autophagy: Autophagy is the body’s natural process of cellular recycling, clearing damaged components. NIASORCINOL™ enhances this process to break down accumulated melanin granules deep within skin cells.
The synergistic effect of these three mechanisms results in faster, more effective brightening with reduced irritation compared to traditional agents like hydroquinone or kojic acid. The innovative design penetrates multiple layers of skin pigment formation and removal, offering a holistic solution to the pigmentation paradox.
Clinical Evidence Supporting NIASORCINOL™ Serum
Clinical studies involving NIASORCINOL™ reveal compelling evidence of its efficacy. Regular use over eight weeks showed substantial reductions in dark spots, dull skin appearance, and visible pores. A majority of users experienced noticeable skin brightness within just two weeks. Importantly, the formulation’s emphasis on tolerability makes it suitable for sensitive skin types prone to irritation from other active ingredients. This clinical validation strengthens NIASORCINOL™’s position as a leading choice for consumers seeking advanced pigmentation solutions.
How to Incorporate NIASORCINOL™ into Your Skincare Routine
To maximize benefits, start with a patch test, especially if you have sensitive skin, applying a small amount to a discreet area for a few days. Once confirmed to be well-tolerated, incorporate the serum twice daily—morning and evening—after cleansing and before moisturizing. Consistent application is key to allowing the active ingredients to support pigment regulation and removal effectively. Complement this routine with broad-spectrum sunscreen use to shield skin from new UV-triggered pigmentation. Combining these steps offers an integrative approach to fading existing spots and preventing their recurrence.
Frequently Asked Questions (FAQs)
1. Can hyperpigmentation be permanently cured?
While dark spots can be significantly lightened, ongoing environmental exposure and skin turnover require maintenance to prevent recurrence.
2. Is niacinamide safe for sensitive skin?
Yes, it strengthens the skin barrier and reduces inflammation, making it suitable for sensitive skin types.
3. How long before I see results?
Visible improvement usually occurs at 4–8 weeks with consistent treatment.
4. Can I sunbathe while treating hyperpigmentation?
No, UV exposure worsens pigmentation and can nullify treatment benefits.
5. What if my pigmentation worsens with treatment?
This may indicate irritation—stop use and consult a healthcare professional.
Conclusion: Empowering Yourself Through Knowledge and Science
Hyperpigmentation arises from a multifactorial interplay within the skin, including UV exposure, hormonal shifts, inflammation, genetics, and aging. Understanding these causes of hyperpigmentation provides the foundation for prevention and effective treatment.
Modern advances like NIASORCINOL™ complex harness deep pigmentation biology to enable faster, safer, and more sustained results. Coupled with daily sun protection and gentle skincare, these innovations empower achieving and maintaining radiant, even-toned skin, restoring confidence and enhancing well-being.